The healthcare industry has long been on the cusp of a digital revolution - and for startups looking to make a real impact, now is the time to act. Building a healthcare software product is no longer just about coding an app or integrating APIs. It's about solving real, human problems in an industry that is highly regulated, incredibly complex, and rapidly evolving.
Designed for startup founders and early-stage innovators, this guide walks you through the end-to-end process of healthcare software product development, from idea validation to regulatory compliance.
The Market Is Ready - Are You?
Healthcare software has entered a period of rapid growth and change. As a highly regulated and stakeholder-heavy sector, healthcare has long relied on bespoke software tailored to complex workflows, regulatory requirements, and sensitive data management. Today, that complexity is becoming an opportunity.
According to recent data from Dimension Market Research, the global healthcare software-as-a-service (SaaS) market is expected to grow from $36.8 billion in 2024 to a staggering $93.4 billion by 2033. That's more than double in less than a decade - and it signals one thing: digital health is no longer a niche.
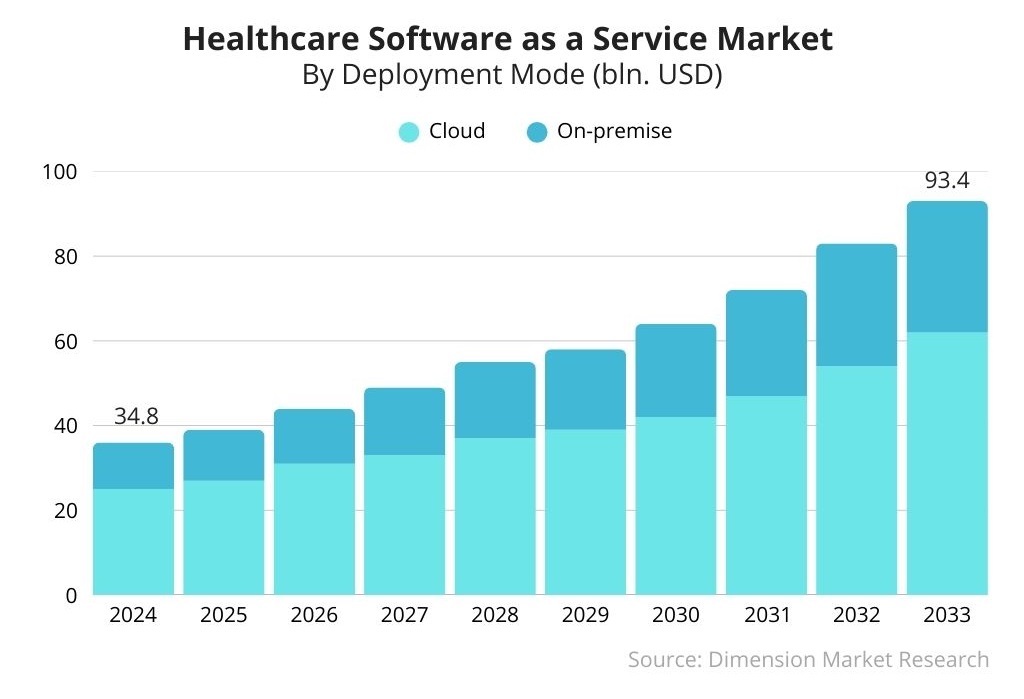
Hospitals, clinics, insurers, and even research labs are actively seeking software tools to streamline operations, reduce costs, and improve care delivery. Much of this transformation is taking place through cloud-based SaaS products - both off-the-shelf and custom-built - that offer scalability, security, and real-time data access.
But it doesn't stop there. A growing number of healthcare solutions are now powered by artificial intelligence (AI) and machine learning (ML), helping decision makers make sense of massive data sets, uncover diagnostic insights, and automate administrative tasks that once required entire departments.
Startups have a clear opportunity: build leaner, faster, smarter products that healthcare organizations are already ready to adopt.
Why Healthcare Needs Your Startup’s Innovation
Healthcare is burdened by legacy systems, administrative inefficiencies, and a chronic underinvestment in digital UX. That's where tech startups come in. The opportunity is huge-whether you're tackling remote diagnostics, chronic disease management, or care coordination, there's room for disruptive digital products.
But success in healthcare software isn't just about launching fast. It's about building right.
Key Factors to Consider Before You Write a Single Line of Code
1. Compliance is Not Optional
From HIPAA (U.S.) to GDPR (EU) to local Ministry of Health guidelines, every region has its own rules. If you’re storing, transferring, or analyzing patient data - even indirectly - your product must comply. Work with legal and compliance experts from day one.
2. Security Is the Core, Not a Feature
Unlike other tech verticals, data breaches in healthcare can literally cost lives - or at least, livelihoods. Your app needs end-to-end encryption, secure cloud infrastructure, granular user permissions, and regular vulnerability audits. Security is part of your product’s value proposition.
3. Interoperability Drives Real Value
Clinics, hospitals, pharmacies, and labs all use different systems. If your product can’t talk to them, it’s going to be left out. HL7, FHIR, and other standards are worth understanding deeply - especially if you’re integrating with Electronic Health Record (EHR) systems.
4. Your UX Must Be Frictionless - for Doctors and Patients
Medical professionals are overloaded and patients may not be tech-savvy. Design with empathy. Onboarding should be instant. Interfaces should feel intuitive. Every click should save time.
5. Plan for Scalability from the Start
Even if you’re building an MVP, your architecture needs to scale. Healthcare usage can spike during crises - or as you get more institutional clients. Use microservices, containerized environments, and plan for long-term maintainability.
Types of Healthcare Software
Healthcare organizations operate through a complex ecosystem of software systems - some visible to patients, others deeply embedded in the backend. For founders entering the space, understanding this ecosystem isn’t optional. It’s your map to identifying product opportunities.
Here’s a deeper look at the major categories of healthcare software, what they do, and how your startup might build for or integrate with them:
1. Electronic Health Records (EHR) & Electronic Medical Records (EMR)
These core systems manage clinical documentation, including patient demographics, medical histories, diagnoses, treatments, allergies, lab results, and imaging data. EHRs are designed for interoperability and sharing across organizations, while EMRs are often internal to a single practice. Startups often integrate with EHRs to augment capabilities like data visualization, analytics, or decision support.
2. Telemedicine & Telehealth Platforms
These tools power remote interactions between clinicians and patients. Telemedicine typically refers to remote diagnosis and treatment, while telehealth includes preventive care, education, and monitoring. Today’s platforms offer synchronous (video, voice) and asynchronous (text, forms, emails) communication, often bundled with appointment scheduling, patient education, and e-prescription features.

Curious how these technologies work in practice? Check out our case study on Salus Telehealth - a robust platform we helped build from the ground up.
3. Practice Management Systems (PMS)
These administrative workhorses help clinics and small practices manage billing, scheduling, documentation, and insurance claims. They often include patient portals or appointment interfaces. A startup offering lightweight modules or automations that plug into existing PMS tools can deliver outsized value.
4. Revenue Cycle Management (RCM) & Billing Solutions
RCM software streamlines the journey from patient intake to payment. That includes eligibility checks, coding, claim submissions, collections, and auditing. Innovations in this space increasingly rely on AI/ML to spot anomalies or predict denials before they happen. Startups that can optimize reimbursement for providers or reduce administrative burden have a strong business case.
5. Patient Portals & Communication Tools
Patient-facing software supports access to health records, lab results, intake forms, reminders, and secure messaging. While often bundled with EHRs or PMS systems, independent tools offer cleaner UX and more flexibility. Founders focused on patient experience can develop white-labeled, mobile-first solutions that plug into clinical systems.

For a real-world example of how streamlined patient engagement can be achieved, check out our Decide Treatment case study - a platform that empowers patients with better access and decision-making tools.
6. Payer Systems
Used by insurers and other healthcare payers, these systems manage member data, plan rules, authorizations, billing, and reimbursements. Though harder to break into as a startup, opportunities exist in optimizing cost prediction, fraud detection, and value-based care metrics.
7. Laboratory Information Systems (LIS)
These manage lab workflows: tracking samples, running diagnostics, and compiling results. LIS platforms are often siloed and legacy-based. Startups focused on lab automation, data integration, or remote diagnostics may find ground here - especially in home health or telehealth partnerships.
8. Remote Patient Monitoring (RPM)
RPM solutions track patient vitals from outside clinical settings using connected devices - e.g., blood pressure cuffs, glucose monitors, or wearables. These tools often feed real-time data back to care teams for proactive intervention. The market is booming, especially for startups focused on chronic condition management.
9. Mobile Health Apps (mHealth)
From fitness trackers to condition-specific coaching platforms, mHealth spans both clinical and consumer-facing tools. Increasingly, hospitals and insurers partner with startups to offer white-label apps that help with medication adherence, care navigation, or lifestyle changes.
10. Clinical Communication & Collaboration Tools
These systems support secure messaging and task coordination among medical staff. Modern versions integrate with EHRs, escalate alerts based on urgency, and route messages to the correct team. Startups that modernize pager-era workflows with mobile-first, HIPAA-compliant solutions are gaining fast traction.
11. ePrescribing Software
Regulated digital tools that allow doctors to send prescriptions directly to pharmacies. These systems must meet national standards (like Surescripts in the U.S.) and ensure medication reconciliation. Startups entering this space need deep compliance knowledge - or can offer auxiliary services such as fraud detection or formulary checks.
12. Staff & Shift Management Tools
Hospitals and large clinics juggle thousands of shifts weekly. Specialized HRM systems help optimize staffing levels, reduce burnout, and control costs. Founders with experience in logistics or workforce automation can bring fresh ideas to this overlooked but critical domain.
Understanding where your product fits - and how it interoperates with these systems - is essential not just for product design, but also for go-to-market planning, pricing, and compliance.
The Development Roadmap
As with any software product, success begins with a solid foundation - not just in code, but in strategy, compliance, and user-centered thinking. Here’s how startup founders can approach healthcare software development from the ground up:
Step 1: Idea Generation
Collaborate with stakeholders, including clinicians, administrators, and patients, to deeply understand the problem you’re solving. Frame it in human terms: what is broken in the current system? What would meaningful improvement look like? Look for functionality gaps in current tools - integration issues, security lapses, or clunky UX - and brainstorm how your product could address them.
Step 2: Identify Protected Health Information (PHI)
Determine whether your app will handle PHI or interact with Health Information Exchanges (HIEs). This will immediately place it under a higher degree of regulatory scrutiny and define the types of data protection and encryption protocols you’ll need from day one.
Step 3: Screen the Idea for Feasibility
Once you’ve validated a meaningful problem, conduct a feasibility assessment with both business and technical leads. Whether working with your in-house team or external development partners, ensure the concept is realistically executable within budget, time, and compliance constraints.
Step 4: Define Features and Functionality
Build a detailed vision document outlining the product’s intended capabilities. This should include a clear list of features for both users and administrators, any API or EHR integrations, privacy measures, and accessibility options. Prioritize what’s essential versus what can wait.
Step 5: Create a Product Roadmap
Organize your features into a product backlog. Decide which features make up your MVP, and plan phased releases for others. The roadmap should align short-term development with long-term business goals - whether scaling into new markets or onboarding new provider types.
Step 6: Design and Prototype
Begin wireframing your solution. Focus on creating a prototype that validates both the UI and UX. Conduct usability testing with real users - not just developers - and begin early compliance and security checks. Can users complete the key workflows? Would they use this instead of their current process?
Step 7: Development and Implementation
Move into development using Agile methodologies. Iterative sprints let you incorporate frequent user and stakeholder feedback. Build incrementally toward a functional MVP, with secure infrastructure, compliance protocols, and audit logs built-in - not bolted on.
Step 8: Testing
Testing isn’t an afterthought in healthcare - it’s core to trust and regulatory approval. You’ll need to run unit, integration, performance, and vulnerability tests - especially if you’re aiming to be HIPAA-compliant. Don’t overlook usability testing either - especially with clinicians who may resist complex new workflows.
Step 9: Launch with a Learn Mindset
Release your MVP into a closed or alpha group, especially if clinicians are the primary users. Use real-world feedback to iterate fast and make informed decisions about deeper workflow integrations. Measure everything - not just usage, but user sentiment and business value.
Step 10: Promotion and Training
If your product is intended for wide rollout, plan for adoption as seriously as you plan for development. Build onboarding flows, create detailed documentation, and offer guided training. Enlist internal champions within provider organizations to support buy-in at the department level.
Step 11: Gather User Feedback
Post-launch, gather feedback continuously from NPS scores and usage metrics to one-on-one interviews. Feed this directly into your backlog and reprioritize future iterations based on what delivers the most impact to users.
Step 12: Maintenance and Support
Healthcare software must remain agile even after launch. Regulatory frameworks shift. New integration demands emerge. Maintain a support infrastructure for bug resolution, security patching, and system upgrades. Modern healthcare products also need a supply chain security strategy, ensuring third-party components remain safe and trusted.
Check out a related article:
Key Types of Healthcare Software with Examples
Want help staying on track? We’ve prepared a detailed product development checklist that helps founders avoid common pitfalls and keep aligned with healthcare standards.
Challenges in Healthcare Software Product Development
Bringing a healthcare software product to life involves more than innovative thinking and good code. It means navigating a complex matrix of regulations, legacy infrastructure, diverse stakeholders, and high-stakes outcomes. Here are some of the primary challenges startup founders should prepare for:
1. Regulatory Compliance
Healthcare software must meet a wide variety of local, national, and international regulations. This includes implementing technical and organizational measures (TOMs) that protect sensitive data and comply with standards such as HIPAA, GDPR, or local equivalents. Regulations also impact how your product is hosted (e.g., cloud compliance), how data is processed, and whether it falls under medical device oversight.
2. Interoperability
Your software won’t exist in a vacuum. Healthcare organizations depend on multiple systems, and those systems must work together. Supporting standards like HL7, FHIR, and others is essential to enabling seamless data exchange and unlocking the full value of your solution.
3. Choosing the Right Tech Stack
The wrong stack can kill your product before it launches. You’ll need a tech stack that’s scalable, secure, and compatible with healthcare infrastructure. It should also allow future integrations with AI and data analytics tools as the market evolves.
4. Operational Constraints
Healthcare software is often mission-critical meaning it must deliver near-perfect uptime. If your users work in low-connectivity environments (e.g., rural clinics, mobile units), offline functionality becomes a non-negotiable.
5. Cultural Resistance to Change
Clinicians are focused on delivering care, not learning new software. Any workflow disruption can lead to pushback. Successful adoption requires early stakeholder involvement, intuitive UX, and phased implementation strategies.
6. Time to Market vs. Institutional Timelines
Healthcare organizations make decisions slowly. Even with a great product, the sales cycle can be long. Founders must manage burn rates and investor expectations accordingly, while building for long-term relevance.
Regulations and Standards Every Founder Must Know
Healthcare software is highly regulated and the complexity only increases depending on the markets you serve and the type of product you offer. Staying informed about legal, security, and privacy requirements is a continuous responsibility.
Key Healthcare Regulations
- HIPAA (U.S.): Requires strict administrative, physical, and technical safeguards for PHI.
- GDPR (EU): Governs the handling of personal data, including health data, across the EU.
- HITECH Act (U.S.): Promotes EHR adoption and enforces stronger security measures.
- FDA CFR 21 Part 11: Applies to electronic records and signatures, particularly for medical devices.
- EPCS: Regulates e-prescriptions for controlled substances in the U.S.
- eIDAS: EU regulation for secure electronic transactions and identity verification.
- CURES Act Final Rule (U.S.): Enhances patient access to electronic health info.
- NSM-22 (U.S.): Mandates risk management for federal health agencies.
- NIS-2 (EU): Introduces mandatory risk management and incident reporting.
- EU Cybersecurity Act: Outlines certification requirements for ICT solutions.
- EO 14028 (U.S.): Executive Order on improving the nation's cybersecurity, impacting software supply chain standards for government vendors.
Standards and Certifications
Beyond laws, various international and industry-specific standards shape how software must be developed, validated, and audited:
- ISO/IEC 27001: Information security management systems.
- HITRUST CSF: Framework aligning healthcare security and compliance.
- FDA Guidance & MDR (EU): For software that qualifies as a medical device.
- NIST Frameworks: Best practices for cybersecurity, especially in U.S.-based systems.
- ENISA Guidelines: European cybersecurity best practices.
Many healthcare entities will require proof of compliance or certifications — especially when onboarding new vendors. It’s worth building your product roadmap with these expectations in mind.
Technologies That Are Changing the Game

Healthcare software development is rapidly evolving thanks to groundbreaking innovations. Here are the most transformative technologies shaping the future of healthtech and how startup founders can take advantage of them:
Artificial Intelligence (AI) & Machine Learning (ML)
AI and ML are no longer buzzwords - they’re becoming foundational. In healthcare, these technologies are already being used to power predictive analytics for population health, automate radiology diagnostics, detect anomalies in medical imaging, and support early disease detection through natural language processing (NLP).
For example, startups like Aidoc use AI to detect urgent medical conditions from CT scans in real time. Founders looking to enter this space can explore use cases like automated triage, clinical documentation support, or personalized treatment planning based on historical EHR data.
Internet of Medical Things (IoMT)
The IoMT connects wearable devices, implantable sensors, and remote monitoring equipment to clinical systems. This allows care teams to collect real-time data on patient vitals, medication adherence, or post-operative recovery - even outside hospital walls.
Use cases include Bluetooth-enabled glucose monitors, smart inhalers, and remote ECG devices. A startup integrating with wearables to manage chronic conditions, like diabetes or heart disease, can offer tremendous clinical and economic value.
Blockchain
Blockchain in healthcare is about more than cryptocurrency. It offers transparent, tamper-proof data exchange, especially valuable in managing longitudinal health records, clinical trial results, and supply chains for medical equipment.
One emerging use case is patient-controlled health data. Through smart contracts, patients could authorize secure, time-limited access to their data across providers. This promotes interoperability and data integrity while putting privacy control in patients’ hands.
Voice Technology
Voice interfaces are transforming healthcare workflows by enabling hands-free documentation, real-time note-taking, and interaction with medical systems - especially valuable in high-intensity settings like emergency rooms or operating theaters.
Tools like Nuance’s Dragon Medical One are already widely adopted for clinical dictation. Startups can apply voice tech to eldercare (voice assistants for medication reminders), remote diagnostics, or multilingual translation for care teams.
Augmented and Virtual Reality (AR/VR)
AR and VR are becoming more prominent in medical training, physical therapy, and even mental health. Surgeons are using AR overlays during complex procedures, while VR is being tested for PTSD and anxiety treatment.
Startups building immersive training tools for medical schools or rehabilitation apps for stroke patients could leverage this tech to provide engaging and clinically proven results.
Robotic Process Automation (RPA)
RPA enables healthcare organizations to automate repetitive tasks like claims processing, data entry, appointment scheduling, or inventory tracking. This improves efficiency and reduces errors freeing up human staff for higher-value work.
Founders developing RPA-powered modules for small practices or telehealth platforms could deliver serious ROI by automating patient intake, referrals, or follow-ups.
Estimating the Costs of Healthcare Software Product Development
The cost of developing healthcare software can vary widely depending on multiple factors and getting an accurate estimate early is crucial for planning and securing funding. Here’s what to consider:
Factors That Influence Development Costs:
- Type of Product: A secure EHR platform will require significantly more investment than an internal workflow tool or wellness app.
- Project Complexity: The number of features, types of users, depth of integrations (e.g., EHR, payment, wearables), and whether features are built from scratch or via third-party libraries all affect cost.
- Security Requirements: Products handling PHI or subject to FDA or CE regulation will need deeper audits, encrypted environments, and risk assessments.
- Hiring Model: Whether you use in-house developers, hire freelancers, or work with an external agency will have significant implications for speed, cost, and quality.
- Infrastructure & Tools: Will your product require dedicated cloud services, DevOps automation, or integration with licensed tools and APIs?
- UX & Market Research: Gathering user insights, running usability tests, and validating design patterns adds upfront cost but reduces downstream risk.
When in-house expertise isn’t enough and off-the-shelf solutions fall short, building custom software becomes the logical choice. At this point, many organizations must decide: develop in-house or outsource?
In-House vs Outsourcing: Strategic Considerations
Below is a comparison table derived from industry best practices and the visual data you provided:
| Criteria | In-House Development | Outsourced Development |
|---|---|---|
| Team Skills | Ideal if internal team has required expertise, though ramp-up may be slow in case of skill gaps | Immediate access to global experts in healthcare software development |
| Project Requirements | Best for highly-integrated or ongoing internal system development | Great for focused projects that don’t need deep integration from day one |
| Cost Considerations | Includes salaries, benefits, hardware/software, and long-term overhead | Lower upfront costs, with flexibility in scaling and skill use |
| Time Considerations | May be slowed by competing internal priorities or hiring needs | Speeds up delivery via flexible, scalable resources and often 24/7 cycles |
| Control & Communication | Close collaboration with stakeholders, suitable for projects needing high-touch management | Works well with defined requirements, structured workflows, and less frequent iteration |
| Security | Full internal control over data and access | Needs clear protocols and compliance processes (e.g. ISO 27001, HITRUST) but can meet or exceed standards |
| Scalability & Flexibility | Harder to scale without adding permanent headcount | Highly scalable with access to broad technology expertise and rapid ramp-up options |
For many startups, hiring a software development outsourcing company offers a more cost-efficient, scalable path - particularly when it comes to launching a first MVP or accelerating go-to-market under budget constraints. However, the decision should always reflect your internal capabilities, risk appetite, and long-term vision.
Choosing the Right Healthcare Development Partner
If you decide to outsource, choosing the right partner is critical. Here’s what to evaluate:
- Technical and Regulatory Expertise: Look for partners with proven experience in healthcare (FHIR, HL7, HIPAA, GDPR) and emerging tech (AI, IoMT, mobile-first apps).
- Case Studies & Reputation: Always request examples of similar projects, and speak with past clients if possible.
- Human-Centric and Agile Process: Your ideal partner will emphasize UX, iterative development, and feedback-driven sprints.
- Security Credentials: Certifications like ISO/IEC 27001 and HITRUST show serious commitment to protecting health data.
- Risk Management: Your partner should offer secure code signing, third-party vetting, robust access controls, and incident response processes.
If you're ready to bring your healthcare vision to life, Intersog is here to help. With more than 20 years of experience building HIPAA-compliant platforms, AI-powered health solutions, and patient-centric mobile apps, we know what it takes to succeed. Let’s talk about your project.
Leave a Comment